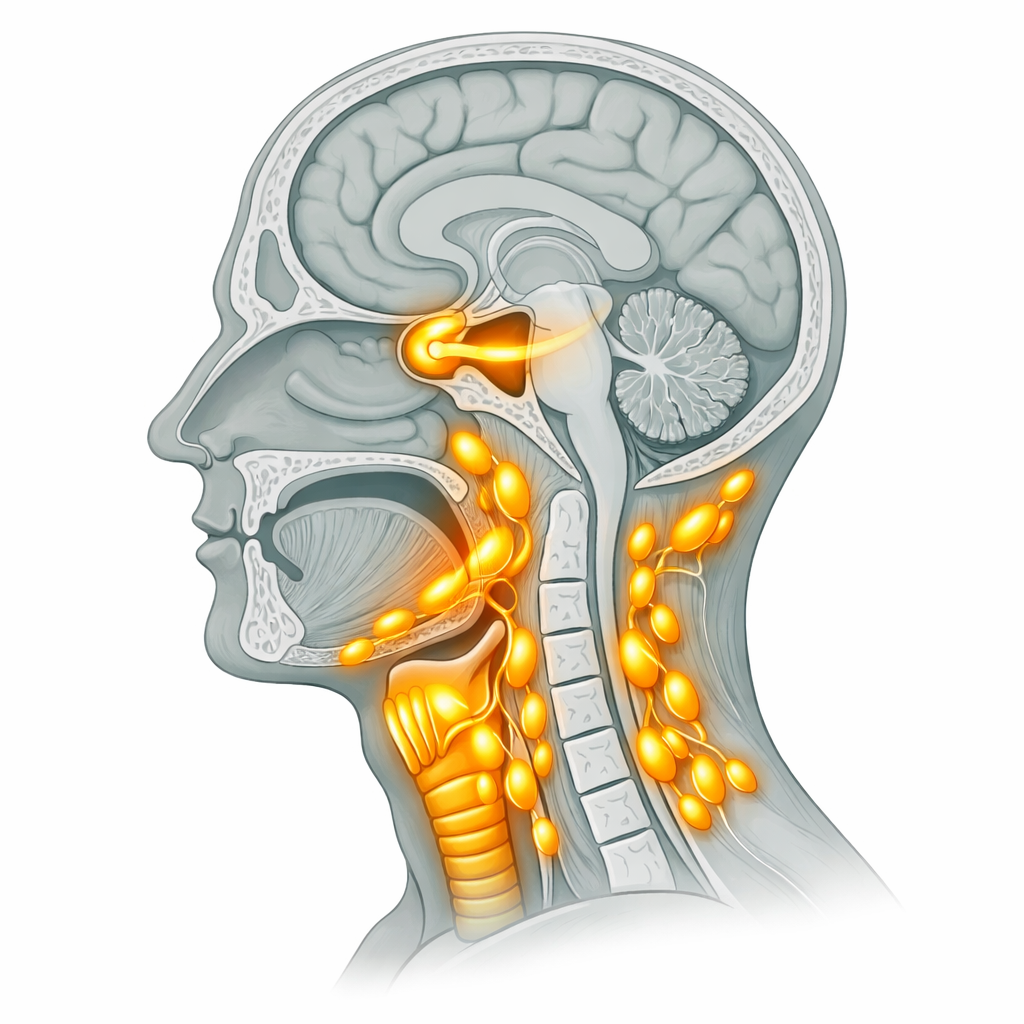
Malaysia is in the headlines again — not for tourism or food, but for tuberculosis. In 2024, the country recorded 26,183 TB cases. As of early 2026, 10 active TB clusters have been confirmed nationwide, with a devastating outbreak in Kota Tinggi, Johor affecting 37 people — including schoolchildren. Experts are now calling it a “slow-burn epidemic.” And as an ENT specialist, here is what concerns us most: many of the earliest warning signs show up in the head and neck — not the lungs.
Most people associate TB with a persistent cough and chest symptoms. That is understandable — pulmonary TB is the most common form. But tuberculosis is a systemic infection capable of affecting almost every tissue in the body. The ear, nose, throat, and neck are among the most frequently involved sites outside the lungs. These are manifestations that get missed, misdiagnosed, and unfortunately, delayed — sometimes for months.
This article is your guide to understanding exactly how TB presents in the ENT region, why it matters right now in Malaysia, and when you should be seeking specialist care rather than waiting it out.
Sources: Ministry of Health Malaysia, Free Malaysia Today, Malay Mail — February 2026
Why TB Is an ENT Problem, Not Just a Lung Problem
Mycobacterium tuberculosis — the bacterium responsible for TB — is spread through the air when an infected person coughs, sneezes, speaks, or sings. It is primarily a respiratory disease, but once it enters the body and the immune system fails to fully contain it, it can travel through the lymphatic system and bloodstream to establish infection almost anywhere.
The head and neck region is particularly vulnerable because it sits directly in the path of inhaled organisms. The upper respiratory tract — your throat, voice box, nasal passages, and middle ear — is the first line of contact. The lymph nodes of the neck drain the tonsils, sinuses, oral cavity, and throat, making them a natural landing point for disseminated TB.
What makes this clinically important is timing: ENT manifestations of TB often appear before the chest symptoms become pronounced, or in cases where the primary lung focus is small and goes undetected on standard chest X-ray. In a country where TB is now described as a slow-burn epidemic, being able to recognise these presentations early is not just good clinical practice — it is potentially life-saving.
The 5 ENT Manifestations of TB You Need to Know
🦴
1. Cervical Lymphadenopathy (Scrofula)
Painless swelling of the neck lymph nodes — the most common form of extrapulmonary TB worldwide.
🎙
2. TB Laryngitis
Persistent hoarseness, voice change, or throat pain caused by TB infection of the voice box.
👂
3. TB Otitis Media
Chronic ear infection with hearing loss and painless ear discharge — often mistaken for a routine middle ear infection.
👃
4. Nasal & Nasopharyngeal TB
Nasal obstruction, bloody or crusted discharge, and post-nasal symptoms from TB in the nasal cavity or nasopharynx.
💊
5. TB Tonsillitis & Pharyngitis
Persistent sore throat, tonsillar enlargement, or ulceration that does not respond to standard antibiotic treatment.
1. Cervical Lymphadenopathy — The Neck Lump That Could Be TB
This is the most important one. Scrofula — TB of the cervical lymph nodes — accounts for approximately 35–50% of all extrapulmonary TB cases globally. In Malaysia, where TB incidence remains high, it is a presentation that every ENT specialist encounters regularly.
The classic presentation is a firm, painless, slowly enlarging lump on the side of the neck, typically in the upper or posterior triangle. What makes it deceptive is that it rarely causes pain in the early stages, so patients delay seeking care. Over weeks to months, the node can soften, develop a fluctuant centre, and eventually rupture to form a chronic skin sinus — a condition known as a “collar-stud abscess.”
Red flags that point toward TB rather than a routine neck lump
⚠️ Seek urgent ENT review if the neck lump has ANY of these features:
- Present for more than 3–4 weeks with no clear cause
- Firm or rubbery in consistency, not tender
- Multiple matted nodes (several nodes stuck together)
- Accompanied by night sweats, unexplained weight loss, or low-grade fever
- Skin overlying the lump has turned bluish-purple or shows thinning
- You have had known contact with a TB patient or live in a high-density setting
- Standard antibiotics have made no difference over 2+ weeks
Diagnosis requires a combination of imaging (ultrasound ± CT neck), and importantly, fine needle aspiration cytology (FNAC) or excision biopsy with TB culture and sensitivity. This is a procedure your ENT specialist can arrange. Do not allow a fluctuant TB node to be simply incised and drained by a general practitioner — this can lead to chronic non-healing sinuses and should be avoided.

2. TB Laryngitis — When Your Voice Is the Symptom
TB laryngitis was historically the most contagious form of TB, with infected patients able to expel enormous quantities of bacteria when speaking or coughing. While it is now less common than in the pre-antibiotic era, it remains clinically significant and is frequently misdiagnosed as acid reflux laryngitis, vocal cord nodules, or even early laryngeal cancer.
In the current Malaysian outbreak context, where schools and close-contact environments are involved, TB laryngitis is worth keeping on your radar — especially if you are a teacher, healthcare worker, or parent in an affected area.
Symptoms of TB laryngitis
🎙 Voice and throat symptoms that may indicate TB laryngitis:
- Progressive hoarseness lasting more than 3 weeks
- Chronic sore throat that does not improve with antibiotics or antacids
- Pain on swallowing (odynophagia), particularly affecting solids
- Sensation of something stuck in the throat
- Coughing with small amounts of blood (haemoptysis)
- Voice fatigue in speakers, teachers, or call-centre staff
Diagnosis is confirmed by ENT laryngoscopy — a quick, in-clinic procedure where a thin flexible camera is used to directly visualise the vocal cords and voice box. Biopsies can be taken if abnormal tissue is seen. TB laryngitis is treatable with the standard anti-TB medication regimen, but early diagnosis is essential to prevent permanent vocal cord damage.
3. TB Otitis Media — The Ear Infection That Won’t Heal
Aural TB — tuberculosis of the middle ear — is rare but represents one of the most diagnostically challenging presentations in ENT. It typically mimics chronic suppurative otitis media (CSOM), an extremely common condition in Malaysia, which means it is almost always misdiagnosed initially.
TB reaches the middle ear most commonly via the Eustachian tube from the nasopharynx, or — less commonly — through the bloodstream. The result is a chronic inflammatory process that destroys the middle ear structures far more aggressively than routine CSOM.
Warning signs that differentiate TB otitis media from routine ear infection
👂 ENT Red Flags — TB of the Middle Ear:
- Painless, persistent, watery (rather than purulent) ear discharge
- Rapidly progressive hearing loss out of proportion to clinical findings
- Multiple small perforations of the eardrum — very unusual in standard CSOM
- Facial nerve palsy alongside ear discharge (indicates aggressive disease)
- Failure to respond to multiple courses of topical and systemic antibiotics
- Granulation tissue in the ear canal on examination
If you or your child has a persistent ear discharge that has not cleared despite 3 or more courses of antibiotic ear drops, please see an ENT specialist rather than repeating the same treatment. TB otitis media requires microbiological confirmation and systemic anti-TB therapy — not just ear drops.
4. Nasal & Nasopharyngeal TB
Nasal TB is rare but real. It typically presents as a long-standing nasal obstruction, crusting, and a bloody or serosanguinous (blood-tinged watery) discharge. On examination, the nasal mucosa may show pale, granular lesions or ulceration. It is most commonly seen in immunocompromised patients, those with HIV co-infection, or in settings of high TB transmission.
More clinically significant in the Malaysian context is nasopharyngeal TB — TB infection of the space behind the nasal cavity. This can mimic nasopharyngeal carcinoma (NPC), which itself has a high incidence in Southeast Asia. Both conditions can present with unilateral ear blockage (due to Eustachian tube involvement), post-nasal discharge, and neck lymphadenopathy.
⚠️ Critical Distinction: Nasopharyngeal TB vs. Nasopharyngeal Cancer
- Both can cause painless neck lumps and unilateral ear blocking
- Both require nasopharyngoscopy and biopsy for definitive diagnosis
- Do not assume either diagnosis without specialist evaluation
- An ENT nasopharyngoscopy is a 10-minute in-clinic procedure and is the only way to tell them apart
5. Persistent Tonsillitis & Pharyngeal TB
TB can infect the tonsils and pharynx (back of the throat), producing a picture that looks deceptively similar to recurrent tonsillitis or peritonsillar abscess. The tonsils themselves may enlarge, ulcerate, or develop whitish patches. Unlike bacterial tonsillitis, TB pharyngitis does not respond to penicillin or amoxicillin — a failure of treatment response is itself a diagnostic clue.
In children — who make up a portion of the current Johor outbreak cases — tonsil involvement should raise particular concern, especially in households or school settings where a TB source case has been identified.

Who Is Most at Risk Right Now in Malaysia?
The Malaysian Ministry of Health has confirmed active clusters in Selangor, Johor, Kedah, Kelantan, Pahang, Perlis, Sabah, and Sarawak. Cases have emerged in boarding schools, workers’ hostels, and household contacts. The people at highest ENT risk include:
🇲🇾 High-Risk Groups in the Current Malaysian Outbreak:
- Schoolchildren and teenagers — particularly in boarding or residential schools in affected states
- Close household contacts of confirmed TB index cases
- Migrant workers living in crowded dormitories or workers’ quarters
- Healthcare workers — frontline staff with repeated exposure risk
- People living with HIV — whose immune systems cannot contain TB as effectively
- Diabetic patients — diabetes is a well-established risk factor for TB progression
- The elderly and those on long-term immunosuppressive medications (e.g., steroids, biologics)
- Individuals who have received a TB diagnosis previously — reactivation is possible
What Should You Do If You Suspect TB in the Head & Neck?
The first and most important message is this: do not self-diagnose, and do not self-treat. TB in the head and neck requires specialist investigation — FNAC, cultures, sensitivities, and sometimes biopsy. Standard blood tests and chest X-rays alone will not rule it out.
Your action plan
✅ Step-by-Step: If You Have ENT Symptoms During Malaysia’s TB Outbreak
- Step 1: See a doctor promptly if you have had any of the ENT red-flag symptoms listed in this article for more than 3 weeks — especially alongside fever, night sweats, or weight loss
- Step 2: Ask for a referral to an ENT specialist — your GP or klinik kesihatan can fast-track this if TB is suspected
- Step 3: Inform your doctor of any known exposure to a confirmed TB patient, or if you live in one of the currently affected states
- Step 4: Do not stop any prescribed TB medication early — partial treatment leads to drug-resistant TB, which is far harder to cure
- Step 5: If you are a close contact of a confirmed case, attend the MOH contact screening promptly — latent TB can be treated before it becomes active

Frequently Asked Questions
❓ Can TB cause a neck lump even if my chest X-ray is normal?
Yes. Extrapulmonary TB — including cervical lymphadenopathy (scrofula) — can occur with a completely normal chest X-ray. In fact, in some patients, especially those who are immunocompetent, the primary lung focus is so small it is invisible on standard imaging. A neck lump with constitutional symptoms (fever, night sweats, weight loss) always warrants ENT evaluation and FNAC regardless of chest X-ray results.
❓ Is TB of the ear or throat contagious?
TB laryngitis is considered highly infectious because the larynx produces aerosols when speaking. TB of the ear and neck lymph nodes carries a lower transmission risk. However, most patients with extrapulmonary TB also have some degree of lung involvement, so infectious precautions (masking, ventilation) remain important until sputum culture results are available.
❓ My child has had a swollen neck gland for over a month. Could it be TB?
A lymph node that persists beyond 4 weeks, particularly in a child who has attended a school in an affected area or had contact with a TB patient, should be evaluated urgently by a paediatric ENT specialist or general paediatrician with experience in TB. The vast majority of persistent neck lumps in children are benign reactive nodes — but in the current Malaysian context, TB must be actively excluded.
❓ How long does treatment for head and neck TB take?
The standard treatment for extrapulmonary TB — including cervical lymphadenopathy, laryngeal TB, and aural TB — is 6 months of anti-tuberculosis therapy (2 months of isoniazid, rifampicin, pyrazinamide and ethambutol, followed by 4 months of isoniazid and rifampicin). Drug-sensitive TB responds well to this regimen. Drug-resistant TB requires longer and more complex treatment under specialist supervision.
❓ Where can I get TB screening in Malaysia?
TB screening is available at all Klinik Kesihatan (government health clinics) nationwide at no cost. If you are a close contact of a confirmed case, the Ministry of Health will contact you for screening. Private ENT clinics and hospitals also offer comprehensive ENT-focused TB evaluation including FNAC, neck ultrasound, nasopharyngoscopy, and laryngoscopy. For an appointment with our ENT specialists, visit theentdr.com/book-appointment.
🔗 References & Further Reading
| Links |
| Neck lump evaluation and FNAC |
| ENT laryngoscopy procedure |
| Book your ENT consultation |
| Ministry of Health Malaysia TB updates |
| WHO Tuberculosis Fact Sheet |


No responses yet