Many patients ask the same question after sinus surgery.
“Doctor, will my sinusitis come back?”
The honest answer is: it can.
Sinus surgery (often endoscopic sinus surgery / FESS) improves drainage and ventilation. It also allows medication to reach deeper into the sinuses. But surgery is not a “once-and-done cure” for many people with chronic rhinosinusitis.
The good news is this: recurrence risk can be reduced a lot when surgery is paired with the right long-term plan.
This article explains why sinusitis returns, who is at higher risk, and what you can do to keep your sinuses calm for the long run.
Why sinusitis can return after surgery
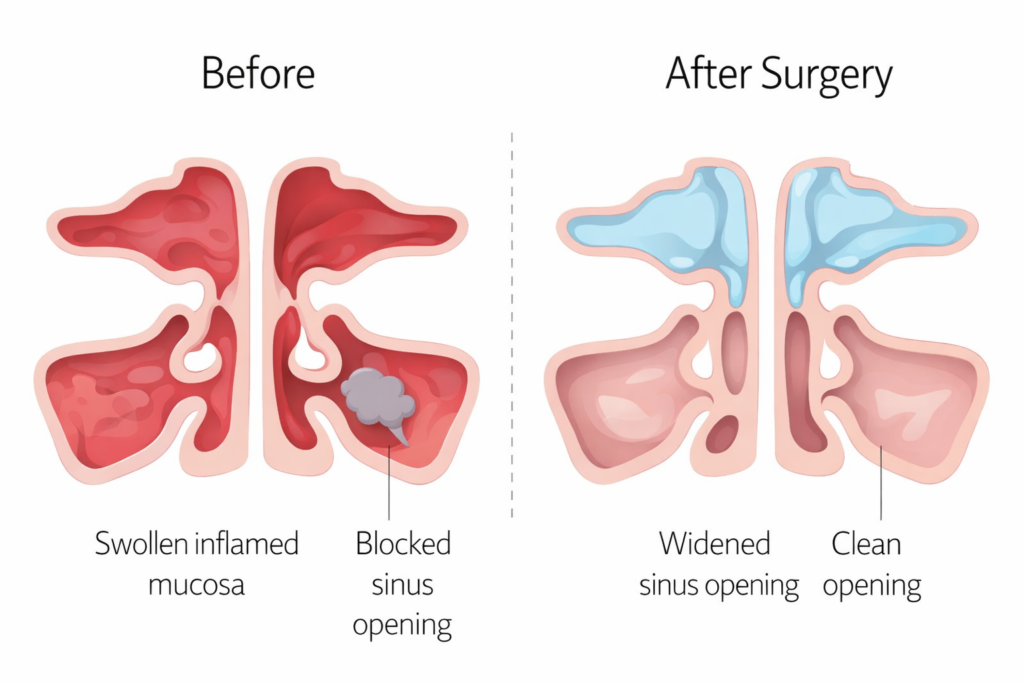
Sinus surgery is like widening a blocked doorway.
It improves access. It improves airflow. It improves drainage.
But the underlying problem in chronic rhinosinusitis is often inflammation, not only blockage.
After surgery, inflammation can still be triggered by things such as:
- Allergic rhinitis (nasal allergy)
- Asthma and “united airway” inflammation
- Nasal polyps
- Ongoing infection or biofilm
- Exposure to smoke or irritants
- Poor nasal hygiene (no rinses)
- Not using anti-inflammatory nasal medication
- Uncontrolled reflux (in selected patients)
- Rare immune problems (in selected patients)
So the best way to prevent recurrence is simple to say, but needs discipline:
Keep inflammation controlled. Keep the sinus openings healthy. Stay on follow-up.
Who has a higher chance of recurrence?
Some patients are more prone to chronic inflammation.
You may be at higher risk if you have:
- Nasal polyps
- Asthma
- Aspirin/NSAID sensitivity (AERD / Samter’s triad)
- Severe allergic rhinitis
- Eosinophilic inflammation (often seen in polyp disease)
- Smoking or vaping exposure
- Frequent sinus infections before surgery
- Poor adherence to rinses/sprays and follow-up visits
Higher risk does not mean surgery “failed”.
It means you need stronger maintenance care after surgery.
What can be done to reduce recurrence after sinus surgery?
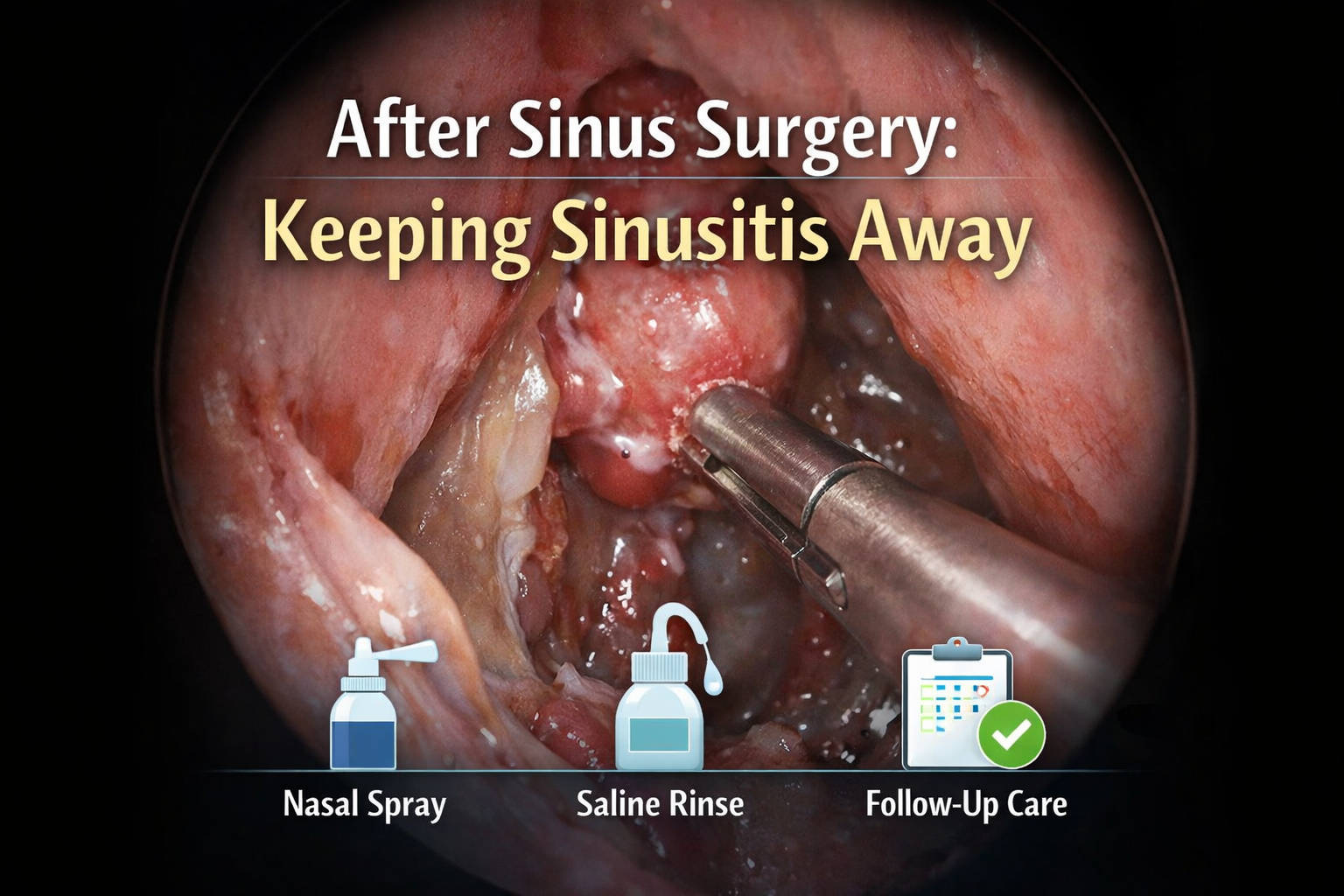
1) Do saline irrigation consistently (this is the big one)

Saline rinsing is not optional after sinus surgery.
It flushes out:
- Thick mucus
- Crusts
- Allergens and irritants
- Residual inflammatory material
It also helps the lining heal in a cleaner environment.
Practical tips
- Use a squeeze bottle or irrigation device (not just a light mist spray).
- Use sterile/distilled water, or boiled-and-cooled water.
- Be consistent. Most patients do best when they make it a routine.
If you only pick one habit, pick this.
2) Use anti-inflammatory nasal medication as prescribed
For many patients with chronic rhinosinusitis, the long-term issue is inflammation.
So the long-term solution often includes:
- Intranasal steroid sprays (maintenance)
- Steroid drops/irrigations in selected cases (especially polyps, guided by your ENT)
After surgery, medication reaches the sinus cavities better. That is one of the main benefits of surgery.
Stopping medication too early is a common reason symptoms creep back.
3) Attend your early post-op visits (cleaning matters)
Early follow-up is not just “checking”.
In many cases, we need to:
- Remove crusts
- Clear trapped mucus
- Reduce adhesions/scarring
- Spot early inflammation before it becomes a full relapse
Think of it like dental scaling after a major gum procedure.
Healing goes better with guided aftercare.
4) Treat nasal allergy properly
Allergic rhinitis keeps the nose inflamed.
Inflammation in the nose often drives inflammation in the sinuses.
If you have sneezing, itch, watery nose, or seasonal flares, talk to your doctor about:
- Daily nasal steroid spray
- Antihistamines when needed
- Allergen avoidance strategies
- Considering allergy testing (in selected patients)
- Immunotherapy (in selected patients)
Controlling allergy is not a “bonus”.
It is part of preventing recurrence.
5) Control asthma and lower airway inflammation
The nose and lungs are linked.
Patients with asthma and sinusitis often flare together.
If your asthma is not controlled, sinus inflammation is harder to control too.
Make sure your asthma plan is optimised with your respiratory physician.
6) Avoid irritants that keep the lining inflamed
If you are exposed to irritants, your sinuses pay the price.
Common triggers include:
- Cigarette smoke and vaping
- Heavy air pollution / haze periods
- Chemical fumes (workplace exposure)
- Strong perfumes and aerosols (in sensitive patients)
Avoiding triggers sounds simple.
But it is often a turning point.
7) Manage reflux if symptoms suggest it
Not everyone needs reflux treatment.
But some patients have significant reflux that irritates the throat and upper airway.
Clues can include:
- Chronic throat clearing
- Persistent cough
- Bitter taste / heartburn
- Hoarseness, especially mornings
If reflux is a contributor, managing it can reduce ongoing irritation.
8) Identify special causes that keep sinusitis coming back
If symptoms keep recurring despite good care, we sometimes look deeper.
Depending on your history, your ENT may evaluate for:
- Dental source of sinusitis (upper molar/root issues)
- Fungal sinus disease (specific subtypes)
- Immune deficiency (rare, but important)
- Structural issues not fully addressed
- Persistent polyps / eosinophilic disease
The goal is to treat the driver, not only the blockage.
9) For nasal polyps: plan long-term maintenance (and newer options exist)
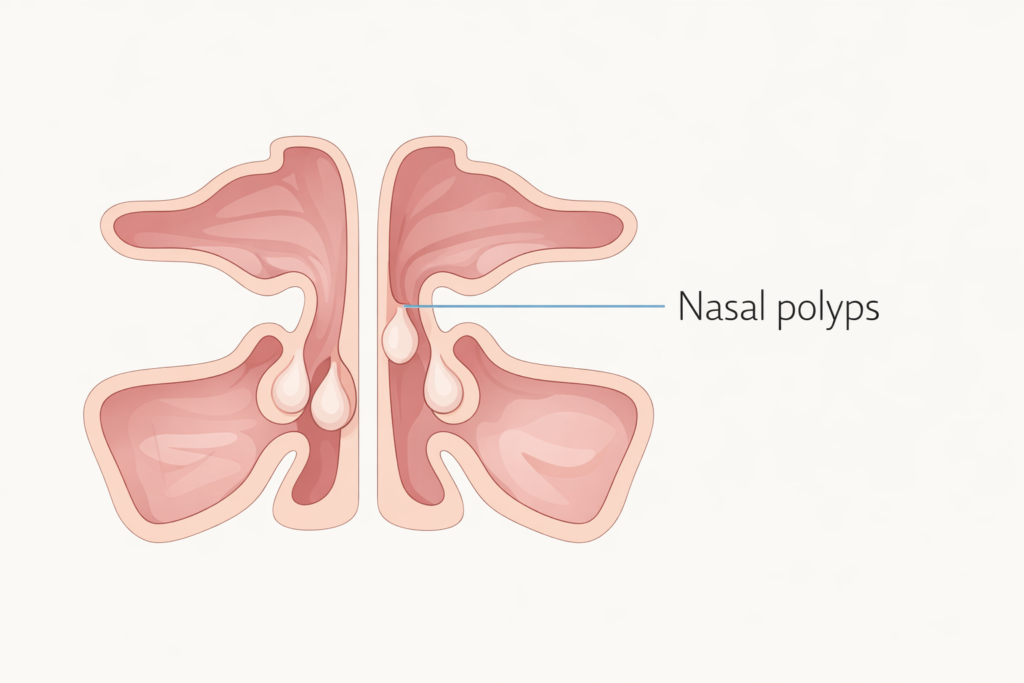
Polyp disease is a “chronic condition”.
Many patients need long-term maintenance to keep polyps small.
Your plan may include:
- Regular saline rinses
- Daily intranasal steroid
- Short courses of oral steroids (only when needed and supervised)
- Management of allergy/asthma
- Aspirin desensitisation in AERD (selected patients, specialised care)
- Biologic injections for severe recurrent polyps (selected patients)
If you have polyps, ask your ENT:
“What is my long-term maintenance plan after surgery?”
That question changes outcomes.

What does “successful surgery” really mean?
A successful operation is not only “a clean scan”.
Success usually looks like this:
- Fewer infections
- Less facial pressure
- Better nasal breathing
- Better sleep
- Better smell (especially when inflammation is controlled)
- Less reliance on repeated antibiotics or steroids
For chronic rhinosinusitis, surgery is often the start of better control, not the end.
A simple checklist to keep sinusitis from returning
Daily / weekly habits
- ✅ Saline rinse (as advised)
- ✅ Use your nasal steroid spray consistently
- ✅ Avoid smoke exposure
- ✅ Treat allergies (don’t ignore “just a bit of sneezing”)
- ✅ Keep asthma controlled if you have it
Follow-up habits
- ✅ Attend early post-op visits
- ✅ Do endoscopic follow-up if symptoms recur
- ✅ Return early when symptoms start (don’t wait months)
When should you see your ENT again?

Book a review if you have:
- Symptoms returning for more than 2–4 weeks
- Frequent flare-ups needing antibiotics
- Reduced sense of smell again
- Persistent thick discharge or post-nasal drip
- New or worsening one-sided symptoms
- Fever, swelling around the eye, severe headache, or vision changes (urgent)
Early treatment is easier than rescuing a late flare.
FAQ
Is it normal to still have mucus after sinus surgery?
Yes, especially during healing. But persistent thick mucus, bad smell, or repeated infections should be assessed.
Can I stop nasal sprays once I feel better?
Many patients can, but many should not. Chronic rhinosinusitis often needs maintenance treatment. Your ENT will tailor this.
Will I need another surgery in the future?
Some patients do, especially those with polyps or severe inflammatory disease. But recurrence risk drops when aftercare is consistent.
Do rinses really make that much difference?
Yes. For many patients, rinsing is the most important long-term habit.
Final message
Sinus surgery creates the pathway.
Long-term control keeps it open.
If you want the best chance of keeping rhinosinusitis from coming back, focus on:
- rinses,
- anti-inflammatory nasal treatment,
- allergy/asthma control,
- trigger avoidance,
- and regular follow-up.
References
- Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020;58(Suppl S29):1–464. doi:10.4193/Rhin20.600.
- Orlandi RR, Kingdom TT, Smith TL, Bleier B, DeConde A, Luong AU, et al. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis (ICAR-RS 2021). Int Forum Allergy Rhinol. 2021. doi:10.1002/alr.22741.
- Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Brook I, Ashok Kumar K, Kramper M, et al. Clinical practice guideline (update): adult sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1–S39.
- Chong LY, Head K, Hopkins C, Philpott C, Burton MJ, Schilder AG. Saline irrigation for chronic rhinosinusitis.Cochrane Database Syst Rev. 2016;CD011995. doi:10.1002/14651858.CD011995.pub2.
- Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
- Chong LY, Head K, Hopkins C, Philpott C, Burton MJ, Schilder AG. Intranasal steroids versus placebo or no intervention for chronic rhinosinusitis. Cochrane Database Syst Rev. 2016;CD011996. doi:10.1002/14651858.CD011996.pub2.
- Tait S, Kallogjeri D, Suko J, Kukuljan S, Schneider J, Piccirillo JF. Effect of budesonide added to large-volume, low-pressure saline sinus irrigation for chronic rhinosinusitis: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2018;144(7):605–612. doi:10.1001/jamaoto.2018.0667.
- Kang TW, Chung JH, Cho SH, Lee SH, Kim KR, Jeong JH. The effectiveness of budesonide nasal irrigation after endoscopic sinus surgery in chronic rhinosinusitis with asthma. Clin Exp Otorhinolaryngol. 2016.
- Green R, Rudmik L. Postoperative nasal debridement following functional endoscopic sinus surgery: a systematic review of the literature. Int Forum Allergy Rhinol. 2015.
- Cochrane ENT Group. Debridement of the nasal and sinus cavities in postoperative care of patients who have had endoscopic sinus surgery. Cochrane Evidence (summary page). 2018.
- Bachert C, Han JK, Desrosiers M, Hellings PW, Amin N, Lee SE, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (SINUS-24 and SINUS-52). Lancet. 2019.

No responses yet