“Weight-Loss Jabs” for Obstructive Sleep Apnea: Help, Hype, or the Real Deal?
You’ve probably heard it already:
“Doc, if I take Ozempic/Wegovy/Mounjaro/Zepbound… will my sleep apnea go away?”
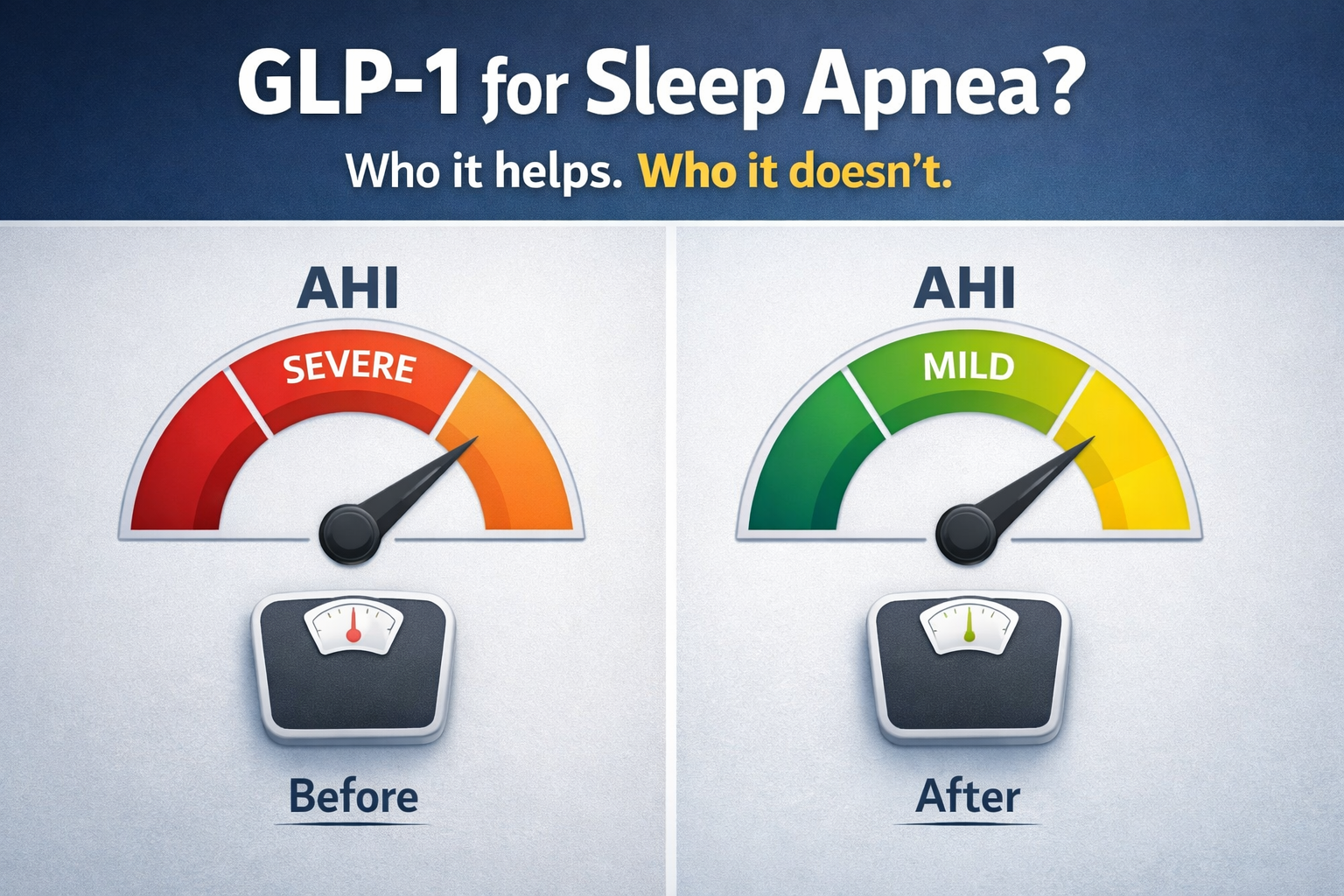
It’s a fair question. Obstructive sleep apnea (OSA) and obesity often travel together. And GLP-1 drugs can cause major weight loss. So it feels logical to connect the dots.
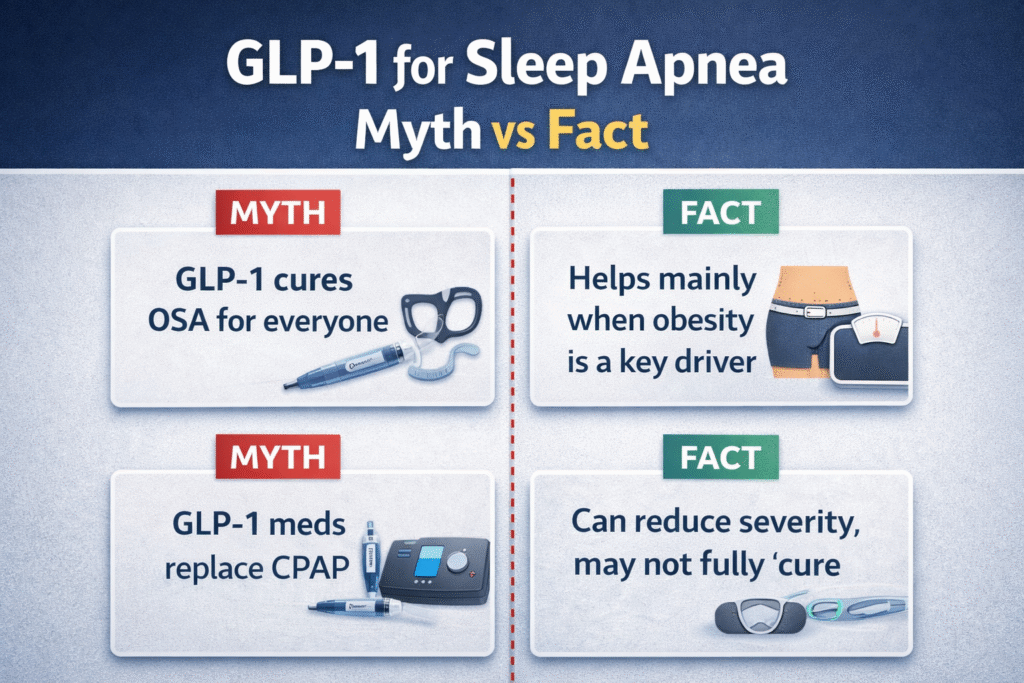
But the real answer is more nuanced:
- GLP-1 drugs can reduce OSA severity in the right patient.
- They are NOT for every OSA case.
- They still require medical supervision.
- They don’t replace a proper sleep apnea plan overnight.
Let’s break it down in a way that’s honest, practical, and safe.
1) What are GLP-1 (and GIP/GLP-1) anti-obesity drugs?
GLP-1 receptor agonists (and newer dual agents) are prescription medications originally developed for diabetes, and now widely used for weight management.
Common examples:
- Semaglutide (e.g., Wegovy/Ozempic)
- Liraglutide (e.g., Saxenda/Victoza)
- Tirzepatide (a dual GIP/GLP-1 agonist; e.g., Zepbound/Mounjaro)
They work mainly by reducing appetite and food intake and slowing gastric emptying (food stays in the stomach longer), which helps people eat less.
Why weight loss can improve sleep apnea (but not always “cure” it)
OSA happens when the upper airway collapses during sleep. Extra body weight can worsen this by increasing fat around the airway and changing airway mechanics.
One key finding: losing weight can reduce tongue fat, and that reduction is strongly linked to improvements in the apnea–hypopnea index (AHI).
So yes—weight loss can meaningfully improve OSA for many people.
But here’s the catch: OSA is not only about weight. Jaw structure, tonsils, tongue position, nasal blockage, and other anatomical factors can drive OSA even in people who are not obese. (More on this below.)
2) What does the evidence say about GLP-1 drugs for OSA?
The “older” GLP-1 evidence: liraglutide (SCALE Sleep Apnea trial)
In a randomized trial (SCALE Sleep Apnea), liraglutide 3.0 mg plus diet/exercise led to a greater reduction in AHIthan placebo in people with obesity and moderate–severe OSA.
This was an early signal that medication-assisted weight loss can improve OSA metrics, not just the number on the weighing scale.
The “big one” for OSA: tirzepatide (SURMOUNT-OSA)
In SURMOUNT-OSA, adults with moderate–severe OSA and obesity had meaningful improvement in AHI with tirzepatide over 52 weeks. One of the trials reported a mean AHI change at week 52 of −29.3 events/hour with tirzepatide vs −5.5 with placebo (treatment difference −23.8).
A clinical summary of the program also notes substantial weight loss in the tirzepatide groups and improvement whether patients were using PAP or not.
Regulatory milestone (US): first medication approved for OSA (specific group)
On Dec 20, 2024, the U.S. FDA approved Zepbound (tirzepatide) for moderate to severe OSA in adults with obesity, used with reduced-calorie diet and increased physical activity.
The American Academy of Sleep Medicine (AASM) stressed an important point: it’s only expected to work for OSA cases related to obesity, and it may not cure OSA because many cases have other causes.
3) Is GLP-1 treatment for every OSA case?
Not for everyone. Here’s the simple rule:
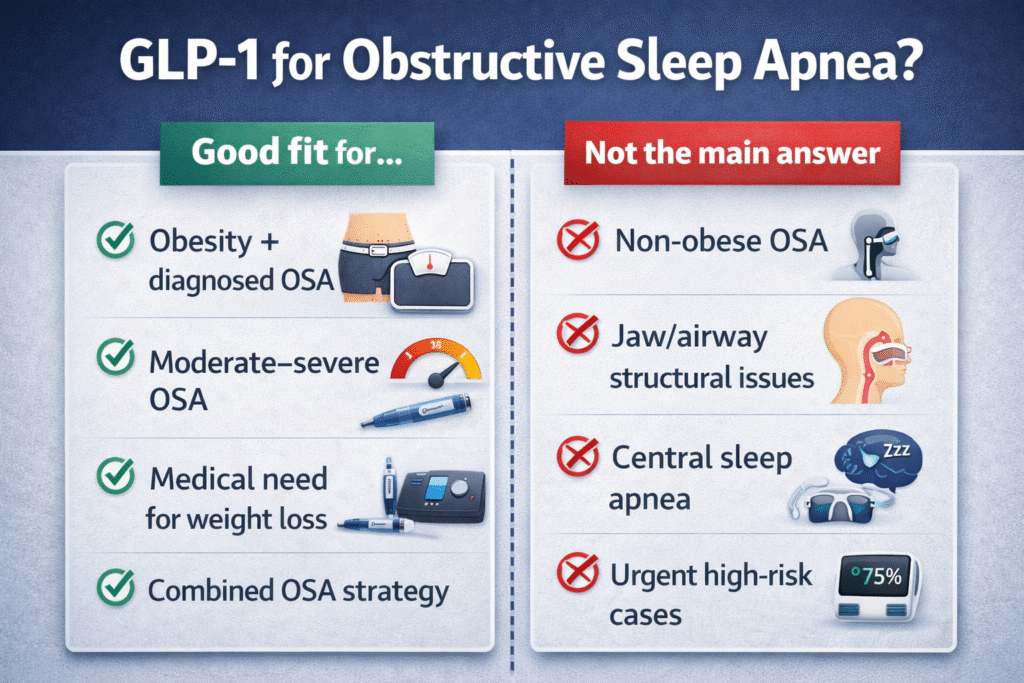
GLP-1 drugs are most relevant when excess weight is a major driver of the sleep apnea.
Likely to help most in these situations
You may be a good candidate to discuss with your doctor if you have:
- Diagnosed OSA (ideally with a sleep study report)
- Obesity (or significant overweight) with weight-related symptoms
- Moderate to severe OSA
- A clear need for medical weight management (especially with diabetes, hypertension, fatty liver, etc.)
- OSA treatment needs that would benefit from a combined plan (e.g., PAP + weight loss strategy)
When GLP-1 is not the right main answer
GLP-1 medication is not a shortcut for OSA that is mainly driven by anatomy or other factors, such as:
- Non-obese OSA
- Major jaw/airway structural issues (retrognathia, narrow upper airway, big tonsils, etc.)
- OSA where the main problem is not weight (AASM specifically highlights this)
- Central sleep apnea (different condition, different treatment logic)
- Urgent high-risk OSA needing immediate control (severe oxygen drops, safety-critical jobs, major symptoms) — you still need a proper OSA treatment plan now, not months later
The truth that surprises people
Even in obesity-related OSA, GLP-1 therapy may reduce severity but not completely “cure” it. Some patients still need PAP, oral appliance therapy, positional therapy, or surgery.
4) Precautions before using GLP-1 drugs (please don’t self-prescribe)
If you take only one message from this post, take this:
Don’t self-prescribe GLP-1 medications. Don’t buy mystery injections online. Don’t copy someone else’s dose.
These are powerful prescription drugs with real contraindications and rare but serious risks.
Before starting, do these basics
- Confirm your diagnosis and severity
- Know your AHI, oxygen drops, and symptoms. (A proper sleep study matters.)
- Assess your “OSA drivers”
- Weight is one driver. Anatomy is another. Many people have both.
- Review contraindications and risks with a clinician
Zepbound (tirzepatide) carries a boxed warning about thyroid C-cell tumors seen in rats, and it’s contraindicated in people with a personal/family history of medullary thyroid carcinoma (MTC) or MEN2.
Semaglutide obesity labels also carry similar thyroid tumor warnings and MTC/MEN2 contraindications. - Plan around procedures / surgery
GLP-1 drugs delay gastric emptying. That can increase the risk of retained stomach contents and aspirationduring anesthesia or deep sedation. Malaysian NPRA safety communications specifically highlight this risk and recommend informing your doctors if you’re on these meds before procedures.
A multisociety perioperative guidance document also focuses on managing aspiration risk (often by identifying high-risk patients and adjusting perioperative plans).
5) Reported major side effects (what people should actually watch for)
Most side effects are gastrointestinal and dose-related, but there are uncommon serious events you should know.
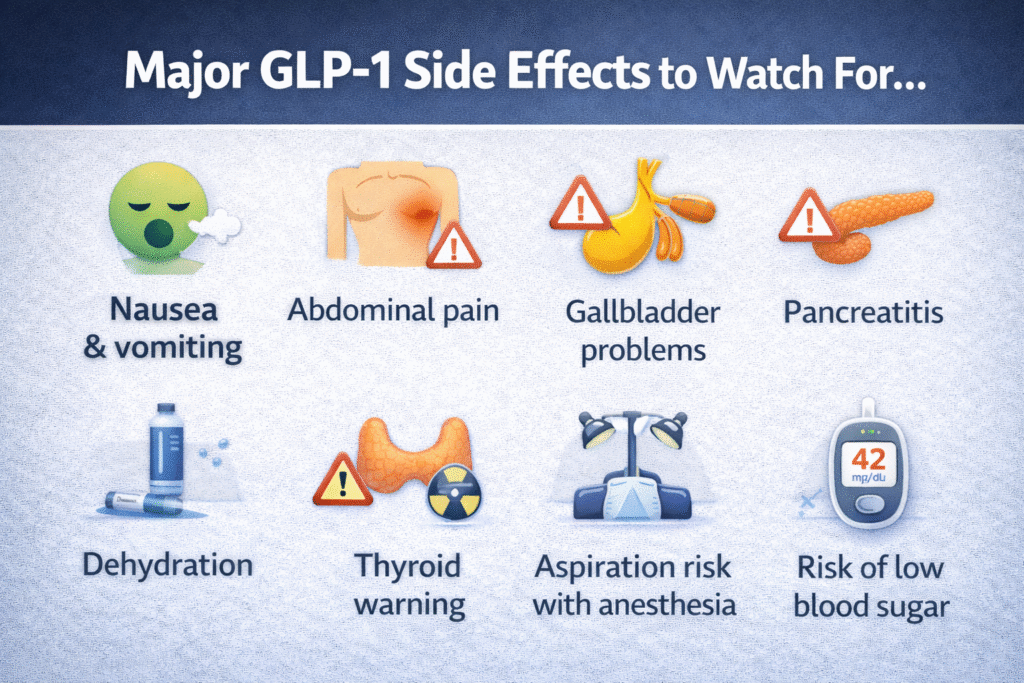
Common (often early, often dose-related)
- Nausea, vomiting, diarrhea, constipation, abdominal discomfort
These are among the most frequently reported adverse events in tirzepatide trials.
Serious or clinically important (seek medical advice urgently)
- Symptoms of pancreatitis (severe persistent abdominal pain ± vomiting) — GLP-1 class warnings include pancreatitis precautions.
- Gallbladder disease (right upper abdominal pain, fever, jaundice) — reported with GLP-1 therapies and discussed in safety reviews.
- Dehydration / kidney injury risk (especially if vomiting/diarrhea is severe) — important to avoid dehydration.
- Hypoglycemia risk when combined with insulin or sulfonylureas (more relevant in diabetes treatment contexts).
- Aspiration risk during anesthesia/sedation due to delayed gastric emptying—tell your surgeon/anaesthetist/endoscopist.
Boxed warning / contraindication highlights
- Thyroid C-cell tumor warning (animal data) and avoid in MTC/MEN2 — appears in prescribing information for tirzepatide and semaglutide obesity indications.
Bottom line: if you’re considering GLP-1 therapy, do it with a qualified clinician who can screen risks, titrate properly, and monitor you.
A practical take: how I’d explain it to a patient in clinic
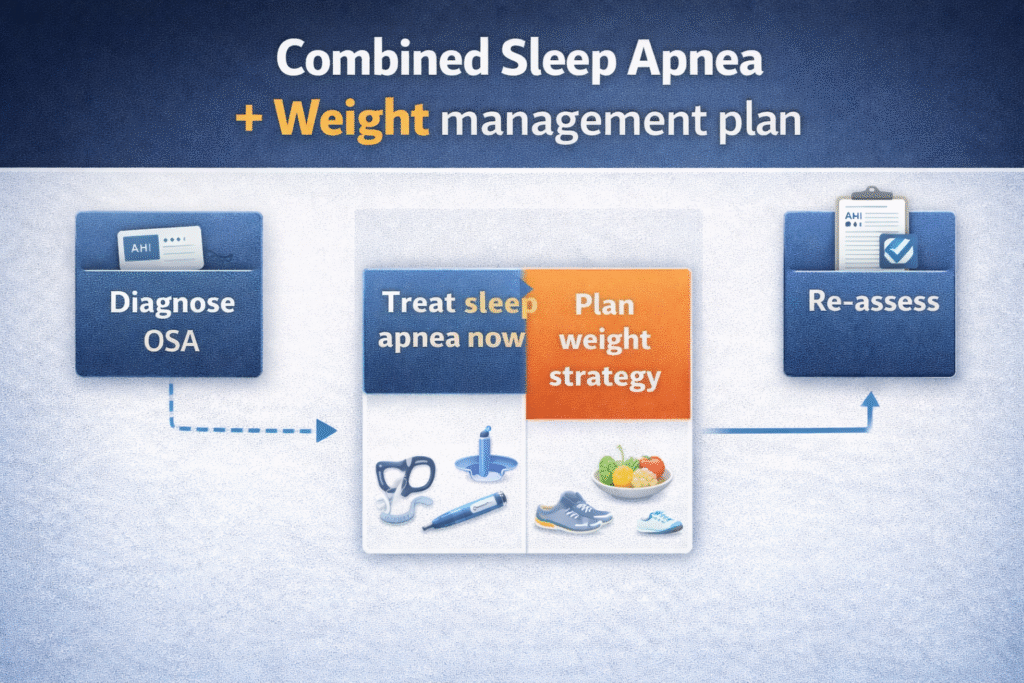
If your OSA is strongly tied to obesity, GLP-1 therapy can be a legitimate add-on tool.
But it should sit inside a real plan:
- Treat the OSA now (PAP, oral appliance, positional therapy, surgery—depending on your case)
- Treat the weight driver long-term (nutrition, activity, behavioral support, medication when appropriate)
- Reassess (repeat sleep testing after meaningful weight change)
And if your OSA is mainly anatomy-driven, we should focus on the airway strategy, not chase weight loss alone.
References (for your own reading)
- U.S. FDA. FDA Approves First Medication for Obstructive Sleep Apnea (Dec 20, 2024).
- Malhotra A, et al. Tirzepatide for the Treatment of Obstructive Sleep Apnea and Obesity (SURMOUNT-OSA). N Engl J Med (2024).
- American Academy of Sleep Medicine (AASM). Statement on Zepbound approval for sleep apnea (Dec 26, 2024).
- Blackman A, et al. Effect of liraglutide 3.0 mg in obesity and moderate/severe OSA (SCALE Sleep Apnea trial) Int J Obes (2016).
- Wang SH, et al. Effect of weight loss on upper airway anatomy (tongue fat) and OSA severity (2020).
- NPRA (Malaysia). GLP-1 receptor agonists: aspiration and aspiration pneumonia during anesthesia/deep sedation (Jan 21, 2025 update).
- Kindel TL, et al. Multisociety perioperative guidance for GLP-1 receptor agonists SOARD (2024).
- Eli Lilly. Zepbound (tirzepatide) U.S. Prescribing Information (PDF).
- U.S. FDA. Wegovy (semaglutide) labeling (PDF).
Discover more from The ENT Doctor
Subscribe to get the latest posts sent to your email.

Comments are closed