“Why did my sleep apnea return after CPAP?”
You start treatment. You feel better. Your partner says the snoring is gone. You wake up clearer.
Then, months or years later, it creeps back.
The tiredness returns. The morning headaches return. The snoring returns. Sometimes it is even worse than before.
This is common. And it does not always mean your treatment “failed”.
It usually means one simple truth:
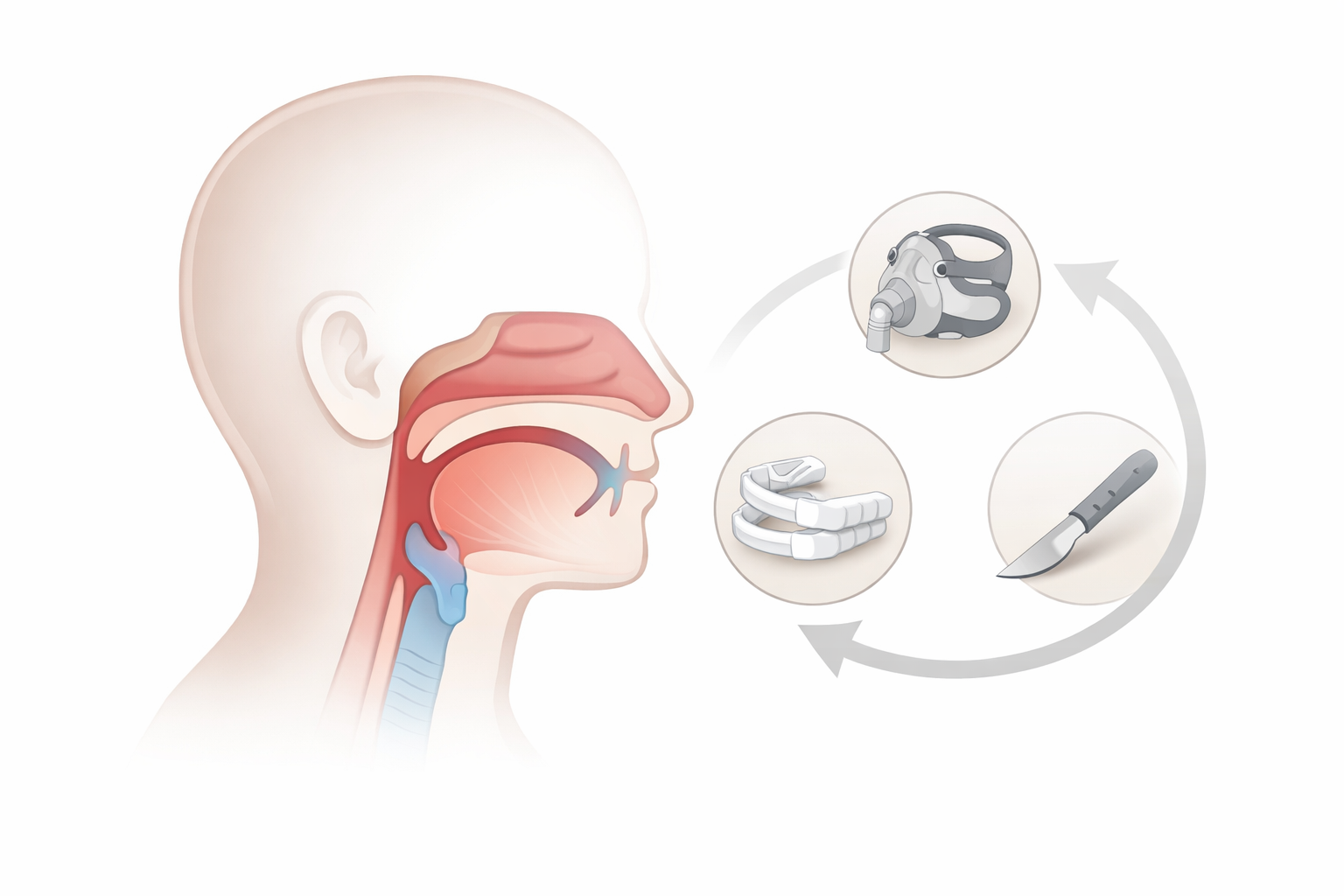
Obstructive sleep apnea (OSA) is a long-term condition. And for many people, it changes over time.
Let’s break down why this happens, and what you should do next.
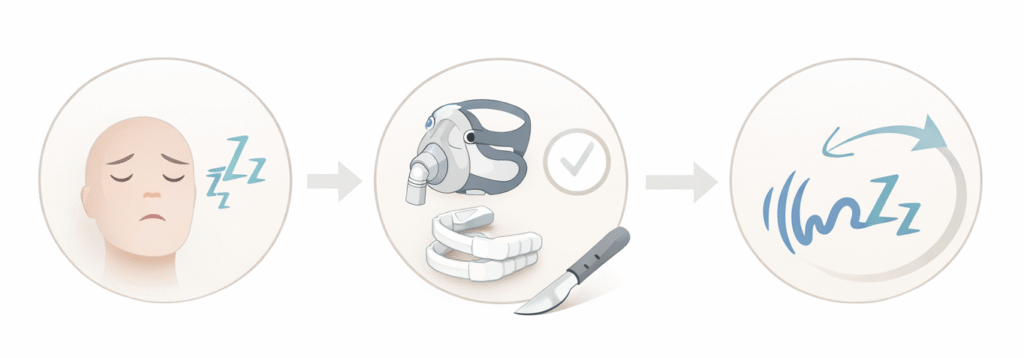
1) “Why did my sleep apnea return after CPAP?”

CPAP is highly effective when it is used well and the settings match your current needs. The problem is that real life gets in the way.
Here are the most common reasons symptoms return:
A. You are not using it enough (even if you think you are)
Many patients gradually use CPAP less over time. Travel. Busy nights. Falling asleep on the sofa. Nasal blockage. Mask discomfort.
Studies consistently show non-adherence is common (often defined as using CPAP less than 4 hours per night).
And here is the hard part:
If you use CPAP for only part of the night, your untreated OSA returns for the rest of the night.
B. Mask leak (silent treatment killer)
A small leak can turn a “perfect” pressure into an ineffective one.
Leaks can be worse when:
- you have nasal blockage
- you gained weight
- you changed mask type/size
- your head position changed
- your facial shape changes with age
Nasal obstruction is a known contributor to unintentional leak.
C. Your pressure needs changed
OSA severity can change. Your airway can become more collapsible. Your required pressure can go up.
Common triggers:
- weight gain
- aging
- alcohol or sedatives
- worsening nasal obstruction (allergic rhinitis, deviated septum, polyps)
- new medical issues (fluid retention, hypothyroid, etc.)
D. “Residual sleep apnea” despite CPAP
Sometimes the machine is on, but events still happen. This can occur when:
- pressure is not optimal
- leaks are significant
- there is mouth leak (especially with nasal masks)
- sleep position worsens (more time on your back)
- another sleep disorder overlaps (insomnia, limb movements)
Bottom line: CPAP problems are often fixable. But you need a proper review and data download.
2) “Why did my sleep apnea return after an oral appliance?”
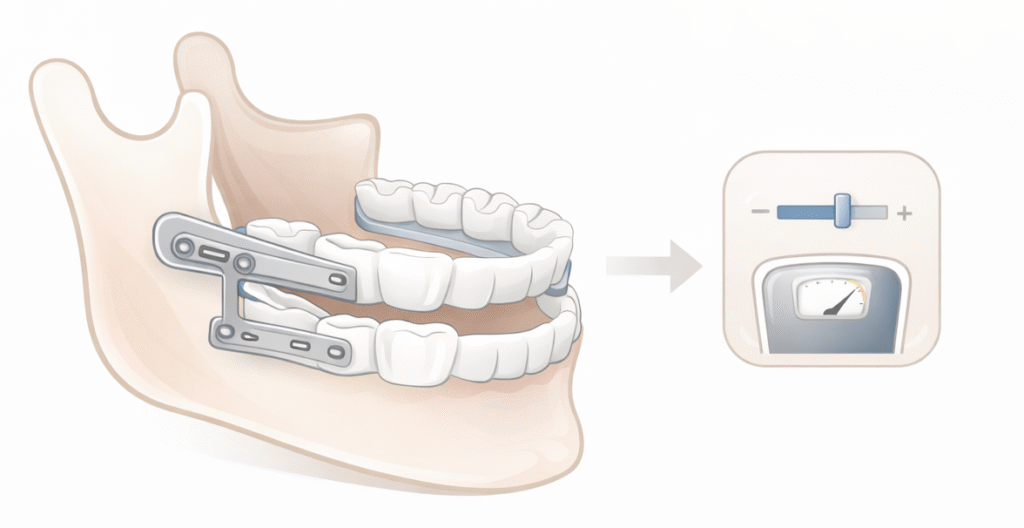
Oral appliances (mandibular advancement devices) can work very well for selected patients. Long-term outcomes can be stable in many people.
But symptoms can return because:
A. The device is no longer advanced enough
Jaw positioning can drift. The appliance may loosen. Your bite can change. Your anatomy changes.
B. Weight gain or aging changed your airway
Even a small weight gain can worsen collapsibility. Obesity is strongly linked to OSA mechanisms.
C. You never confirmed effectiveness with a sleep study
Feeling better is good. But it is not the full picture.
The American Academy of Sleep Medicine recommends follow-up and considers repeat sleep testing, especially if symptoms recur or weight changes occur.
If your symptoms return on an oral appliance, don’t guess. Re-test.
3) “Why did my sleep apnea return after surgery?”
This surprises many patients.
Surgery can be life-changing. But most OSA surgeries are not a “one-and-done cure” for everyone.
Why recurrence happens:
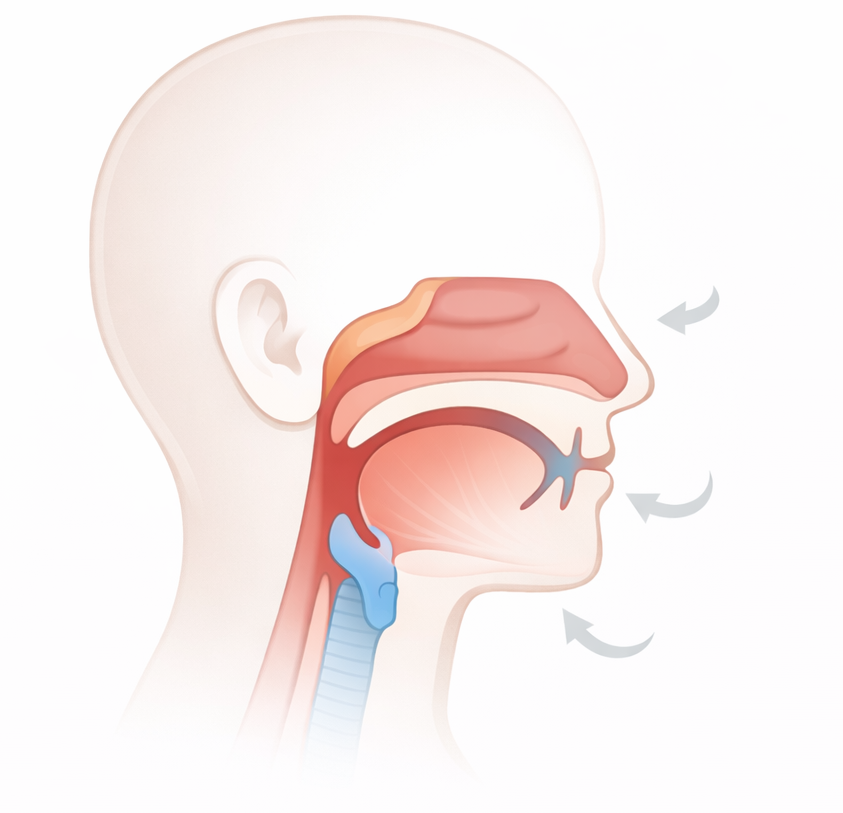
A. OSA is often multi-level
The collapse may involve:
- nose
- soft palate
- tonsils/lateral walls
- tongue base
- epiglottis
If surgery addressed one main area, another area can become the new weak link later.
B. Your body changes after surgery
Common reasons:
- weight gain after initial improvement
- aging and reduced muscle tone
- new nasal blockage
- change in sleep position habits
- progression of comorbidities
C. The airway pattern can shift over time
Your collapse pattern at 35 is not always the same at 45.
That is why long-term follow-up matters, especially if symptoms come back.
4) OSA is a progressive disease. It needs long-term follow-up.
OSA is not like a throat infection. It is closer to high blood pressure or diabetes.
It can improve with the right treatment.
But it can also worsen again if underlying drivers worsen.
And diagnostic testing is not meant to be a one-time event without follow-up. Sleep evaluation and testing should occur with adequate follow-up.
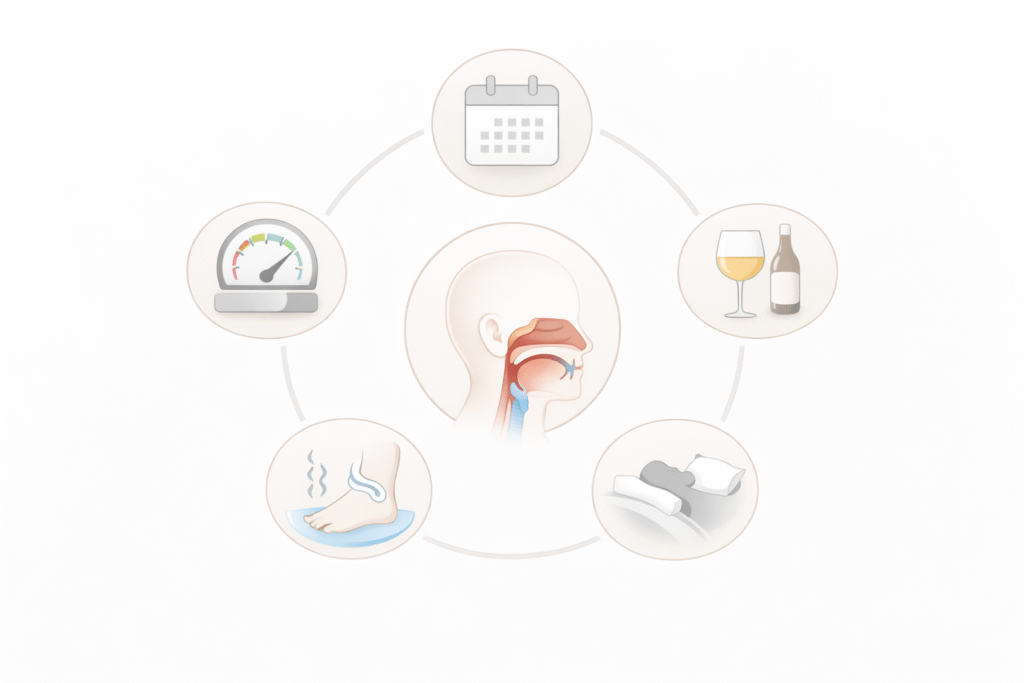
5) Why does OSA progress?
In simple terms: your airway becomes easier to collapse.
Common drivers include:
A. Weight gain and central fat
Fat around the neck and airway increases collapsibility.
B. Aging
With time, muscle tone and reflexes that keep the airway open can weaken. Anatomy and sleep structure change.
C. Nasal obstruction (often ignored)
Chronic rhinitis, turbinate swelling, sinus issues, or a deviated septum can worsen mouth breathing, increase CPAP leak risk, and reduce tolerance.
D. Alcohol, sedatives, and sleep deprivation
These reduce airway tone and worsen collapse.
E. Fluid shift / medical comorbidities
Some conditions increase airway swelling or collapsibility (for example, fluid retention states).
The key message: treatment is not only “choose CPAP vs surgery vs oral appliance.”
It is also “manage the drivers that keep changing.”
6) What should you do if treatment becomes ineffective or symptoms worsen?
Use this checklist. It is practical. It works.
Step 1: Don’t just tolerate it. Don’t self-adjust blindly.
If you feel sleepy again, snore again, or wake up choking again, treat it as a signal.
Step 2: Check the basics (this fixes a lot)
If you are on CPAP:
- Are you using it every night, the whole night?
- Is there mask leak?
- Do you wake with a dry mouth (mouth leak)?
- Is your nose blocked at night?
- Have you gained weight since you started?
Ask for a CPAP data review (usage hours, leak, residual AHI). This is often more useful than guessing.
Step 3: Reassess the diagnosis and current severity
If symptoms recur or worsen, consider:
- repeat home sleep apnea test or polysomnography
- pressure re-titration (CPAP/APAP/BiPAP depending on findings)
- oral appliance re-titration and objective re-testing
For oral appliance patients, AASM guidance supports follow-up and follow-up testing to confirm or reassess effectiveness, especially when symptoms recur or weight changes occur.
Step 4: Look for the “new problem”
Common “new problems”:
- nasal obstruction (treatable)
- weight gain
- new medications that worsen sleep breathing
- positional worsening (more time sleeping on your back)
- alcohol near bedtime
- untreated insomnia reducing CPAP tolerance
Step 5: Escalate or combine treatments if needed
Options may include:
- mask/interface change
- humidification optimization
- positional therapy
- weight management plan
- combination therapy (CPAP + oral appliance, or surgery + CPAP, etc.)
- reassessment for targeted surgery if anatomy has changed
Step 6: Know when it is urgent
Seek help quickly if you have:
- drowsy driving or near-miss accidents
- severe daytime sleepiness affecting work safety
- uncontrolled blood pressure
- new chest pain, palpitations, or stroke symptoms
A simple way to think about it
Your treatment is like a prescription.
But your airway is not static.
So you don’t just “start CPAP” and disappear for 5 years.
You start, you stabilise, and you follow up.
FAQ
Can sleep apnea come back even if I’m still using CPAP, Surgery Or Oral Appliance?
Yes. Treatment adjustments and alternatives may be provided by your care provider
Do I need another sleep study?
If symptoms return, if you gained weight, or if your therapy no longer feels effective, repeat testing is often helpful to guide the next step.
Is sleep apnea “curable”?
Some patients can reach remission (especially with major weight loss or very targeted anatomy). Many need long-term management and follow-up.
References
Correa EJ, Conti C, Piva A, et al. Role of nasal surgery in adult obstructive sleep apnea: a systematic review. Sleep Sci. 2024. doi:10.1055/s-0044-1782527.
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263–276.
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, et al. Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med.2015 Jul 15;11(7):773–827. doi:10.5664/jcsm.4858.
Schwab RJ, Badr SM, Epstein LJ, Gay PC, Gozal D, Kohler M, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med.2013;188(5):613–620. doi:10.1164/rccm.201307-1282ST.
Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008 Feb 15;5(2):173–178. doi:10.1513/pats.200708-119MG.
Reiter J, Zleik B, Bazalakova M, Mehta P, Thomas RJ. Residual events during use of CPAP: prevalence, predictors, and detection accuracy. J Clin Sleep Med. 2016 Aug 15;12(8):1153–1158. doi:10.5664/jcsm.6056.
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015–3021.
Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol (1985). 2005 Oct;99(4):1592–1599. doi:10.1152/japplphysiol.00587.2005.
Yu M, Li M, Dong L, Rueschman M, Li G, Malhotra A, et al. Long-term efficacy of mandibular advancement devices in the treatment of adult obstructive sleep apnea: a systematic review and meta-analysis. PLOS ONE.2023;18(11):e0292832.
Janson C, Gislason T, Bengtsson H, Eriksson G, Lindberg E, Lindholm CE, et al. Long-term follow-up of patients with obstructive sleep apnea treated with uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg.1997;123(3):257–262. doi:10.1001/archotol.1997.01900030025003.
Boyd SB, Walters AS, Waite P, Harding SM, Song Y, Long C, et al. Long-term effectiveness and safety of maxillomandibular advancement for treatment of obstructive sleep apnea. J Clin Sleep Med. 2015;11(7):699–708. doi:10.5664/jcsm.4838.
Heo SJ, Park CM, Kim JS. Time-dependent changes in the obstruction pattern during drug-induced sleep endoscopy. Am J Otolaryngol. 2014 Jan–Feb;35(1):42–47. doi:10.1016/j.amjoto.2013.08.017.

Comments are closed