Does a pillow help treat sleep apnea and snoring?

People ask this all the time:
“If I buy the right pillow… can I fix my snoring or sleep apnea?”
Here’s the honest answer.
A pillow can sometimes help snoring.
A pillow can sometimes reduce sleep apnea severity in a specific subgroup (usually mild-to-moderate, position-dependent OSA).
But a pillow does not “treat” obstructive sleep apnea in the way CPAP treats it, and it’s not a safe “DIY cure” if your OSA is moderate to severe.
Let’s break it down in plain language.
Snoring vs sleep apnea: same family, not the same problem
Snoring is vibration of soft tissues (soft palate, tongue base, etc.) when air squeezes through a narrowed airway.
Obstructive sleep apnea (OSA) is when the airway narrows or collapses enough to cause repeated breathing pauses(apneas/hypopneas), oxygen dips, and sleep disruption.
You can snore without OSA.
You can have OSA without loud snoring.
That’s why “my snoring improved” is not the same as “my sleep apnea is treated.”
How pillows could help (the real mechanism)
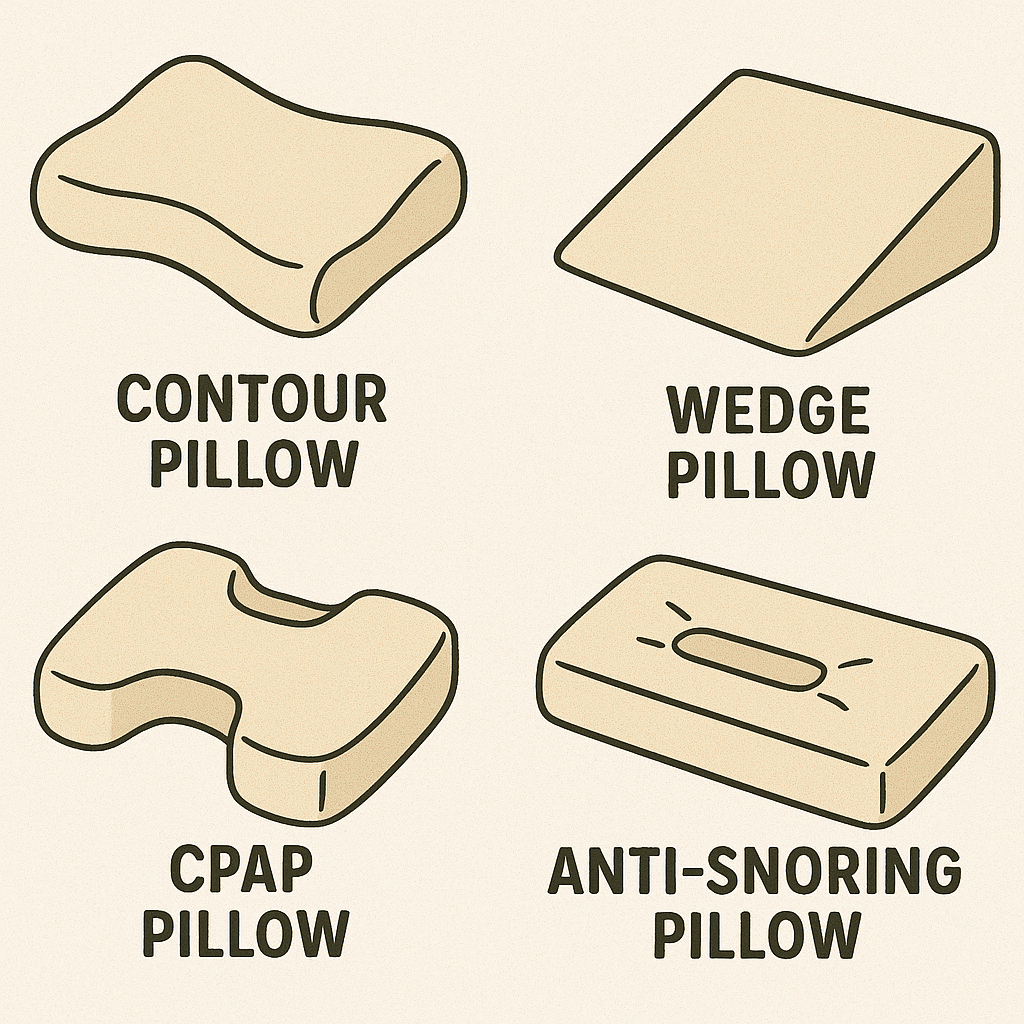
Most “anti-snoring” pillow logic falls into one of these buckets:
1) Keeping you off your back (positional therapy)
Many people obstruct more when sleeping supine (on the back). A pillow can be used as a simple “block” so you stay on your side.
This is real medicine. It’s called positional therapy.
A Cochrane review summary notes positional therapy improves AHI compared with no treatment, but CPAP improves AHI more than positional therapy.
2) Raising your upper body (head-of-bed elevation / wedge)
Elevation can reduce fluid shift toward the neck and can reduce airway collapsibility in some people.
In one clinical study, a mild 7.5° head-of-bed elevation reduced AHI on average (about 31.8%) in patients with predominantly mild-to-moderate OSA, and improved minimum oxygen saturation.
3) Improving head/neck position (cervical “alignment” pillows)
Some pillows aim to stop the head/neck from falling into positions that worsen obstruction (or snoring).
In a Scientific Reports study on positional OSA with snoring, a head-positioning pillow approach (positional therapy) improved snoring-related outcomes and was studied as a positional strategy in that subgroup. Nature
4) “Smart” pillows that nudge you when you snore
These attempt a gentle positional correction.
A pilot study of a smart anti-snore pillow found improvements in snoring measures and AHI in mild-to-moderate OSA, but not in severe OSA.
What the science says (in practical terms)
Pillows can reduce snoring in some people
A preliminary randomized study (Frontiers in Medicine) compared pillow types during PSG and reported that a memory foam pillow was associated with a significant reduction in snoring events (~47%) compared with a generic lab pillow in one group.
That’s encouraging for “snoring-as-a-symptom.”
But it doesn’t automatically mean OSA is fixed.
Pillows can reduce OSA severity in some people (usually mild–moderate)
A classic crossover study compared a shoulder-head elevation pillow vs CPAP in mild–moderate OSA. The pillow reduced average AHI (from ~27 to ~21), but CPAP reduced it far more (to ~5).
So yes—some improvement is possible. But the average effect is smaller than CPAP.
Positional therapy works, but it’s not equal to CPAP for most people
A Cochrane review summary and an AAFP evidence summary both report the same pattern:
- Positional therapy improves AHI and sleepiness vs no treatment.
- CPAP improves AHI more than positional therapy, although some patients may use positional therapy for longer during the night (adherence).
Who is most likely to benefit from “pillow therapy”?
A pillow strategy is most reasonable when someone has:
- Mild OSA, or
- Positional OSA (much worse on the back), or
- Problem snoring (with no red flags), and they want a low-risk trial.
If the patient’s events are largely positional, positional therapy tools (including pillows) can be a legitimate second-line or add-on approach. AAFP
Who should NOT rely on a pillow
Do not let a pillow be the “treatment” if you have:
- Moderate–severe OSA (or you strongly suspect it)
- Significant daytime sleepiness (especially if driving)
- Uncontrolled hypertension, heart disease, stroke history, or atrial fibrillation concerns
- Witnessed apneas + choking/gasping + morning headaches
For these patients, pillows can be an add-on, but not the main plan. PAP therapy is strongly recommended in many symptomatic adults and should be based on an objective diagnosis and follow-up monitoring. PMC
The “viral” truth: 5 myths people keep believing
Myth 1: “An anti-snore pillow cures sleep apnea.”
It can help some positional cases. It does not reliably normalize AHI like CPAP can. PubMed+1
Myth 2: “If snoring improves, apnea is gone.”
Snoring can drop even when apnea persists.
Myth 3: “More pillows = better.”
Too much neck flexion can worsen obstruction in some people.
Myth 4: “Smart pillows work for everyone.”
Evidence suggests benefit mainly in mild–moderate, not severe OSA. PMC
Myth 5: “CPAP is optional if you found the right pillow.”
Guidelines still recommend PAP for many adults with OSA symptoms and risk. JCSM
How to try a pillow approach safely (without fooling yourself)
If you want a practical, low-risk home trial:
- Pick one change at a time
Side-sleeping support or head-of-bed elevation. Not everything at once. - Avoid stacking pillows just under the head
Too much neck flexion (“chin-to-chest”) can worsen obstruction for some people. - If elevating, elevate the upper body
A wedge under the torso is different from extra pillows under the head. In the head-of-bed elevation study, a modest incline (7.5°) was used. - Track symptoms for 2 weeks
Snoring reports, morning headache, dry mouth, daytime sleepiness. - If symptoms persist, don’t guess—test
Home sleep apnea testing or lab PSG is the clean way to know if OSA is controlled.
Bottom line
- Pillows can help snoring, especially if snoring is position-related.
- Pillows can reduce AHI in some mild–moderate cases, particularly with head-of-bed elevation or positional strategies.
- Pillows do not replace CPAP for most people with clinically important OSA.
- If you suspect OSA, the safest move is still: confirm diagnosis, then treat properly.
References
- Patil SP, Ayappa IA, Caples SM, et al. Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2019;15(2):335–343. doi:10.5664/jcsm.7640
- de Barros Souza FJ, Genta PR, de Souza Filho AJ, et al. The influence of head-of-bed elevation in patients with obstructive sleep apnea. Sleep Breath. 2017;21(4):815–820. doi:10.1007/s11325-017-1524-3
- Skinner MA, Kingshott RN, Jones DR, et al. Elevated posture for the management of obstructive sleep apnea. Sleep Breath. 2004;8(4):193–200. doi:10.1007/s11325-004-0193-1
- Chen W-C, et al. Treatment of snoring with positional therapy in patients with positional obstructive sleep apnea syndrome. Sci Rep. 2015;5:18188. doi:10.1038/srep18188
- Chung T-T, Lee M-T, Ku M-C, et al. Efficacy of a smart antisnore pillow in patients with obstructive sleep apnea syndrome. Behav Neurol. 2021;2021:8824011. doi:10.1155/2021/8824011
- Stavrou VT, Astara K, Vavougios GD, et al. Memory foam pillow as an intervention in obstructive sleep apnea syndrome: a preliminary randomized study. Front Med. 2022;9. doi:10.3389/fmed.2022.842224
- Srijithesh PR, Aghoram R, Goel A, Dhanya J. Positional therapy for obstructive sleep apnoea. Cochrane Database Syst Rev. 2019. (Summary page) Cochrane
- Clebak KT, Demetriou TJ, Carey S. Positional therapy for obstructive sleep apnea (Cochrane for Clinicians summary). Am Fam Physician. 2020;101(1):16–17.


Comments are closed